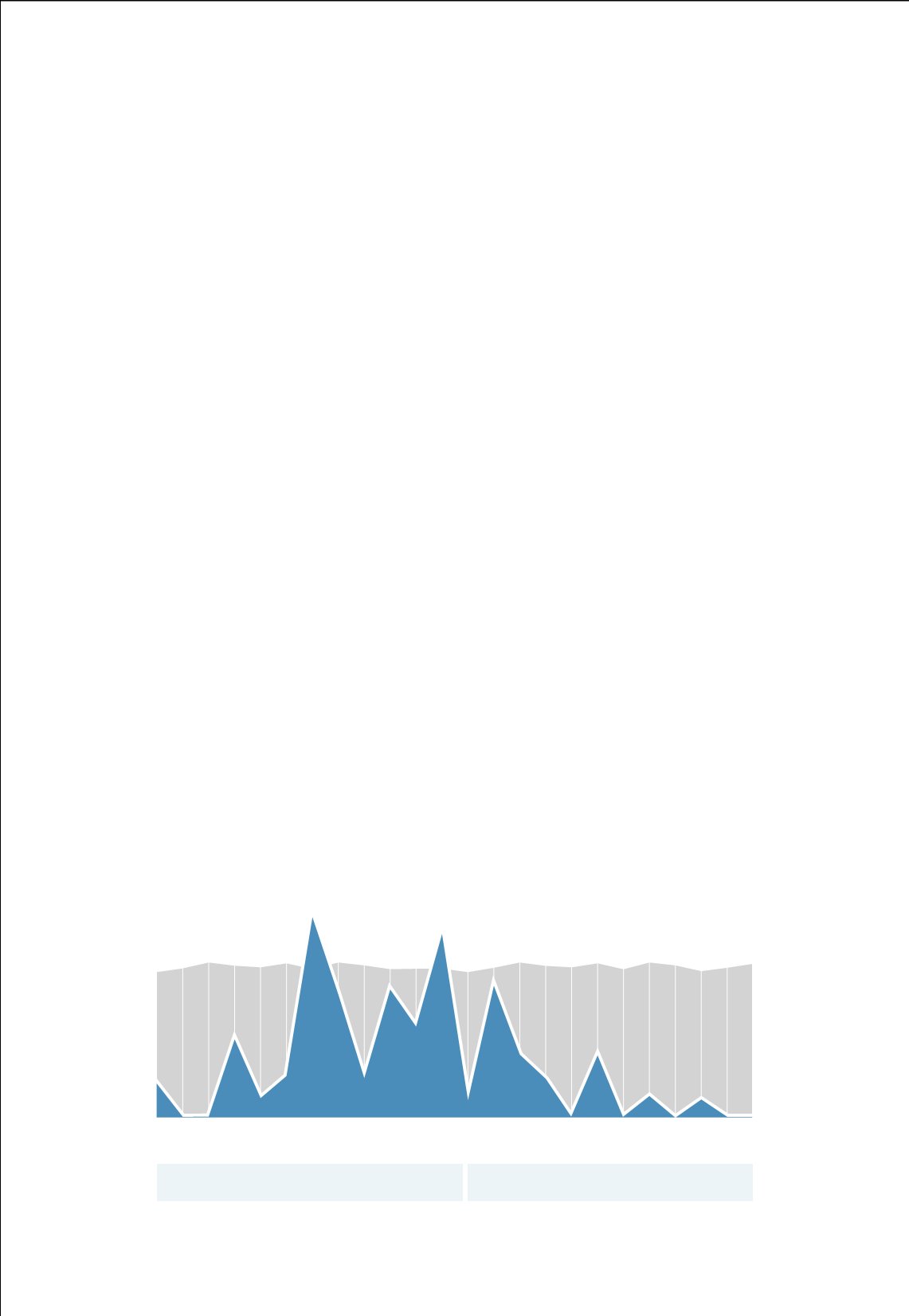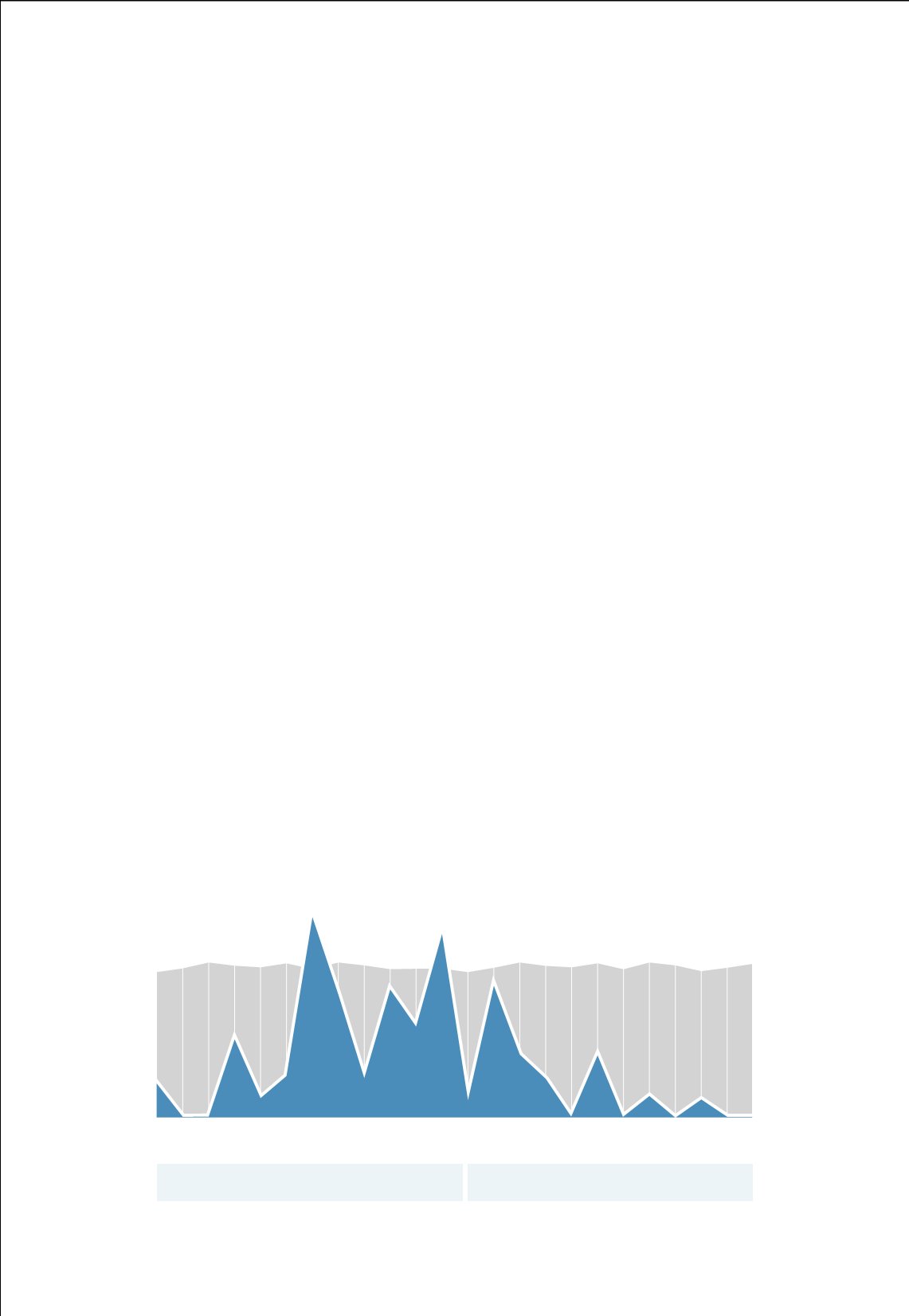
JAN
FEB
MAR
APR
MAY
JUN
JUL
AUG
SEP
OCT
NOV
DEC
JAN
FEB
MAR
APR
MAY
JUN
JUL
AUG
SEP
OCT
NOV
DEC
2012
2013
R AT E /10 0 0 PAT I ENT DAYS
UCL
0
2
4
6
8
10
12
14
16
18
2012-2013
E P I L E P S Y MON I T O R I N G U N I T
H O S P I T A L A C Q U I R E D P R E S S U R E U L C E R R A T E
When Mullen first encountered the problem, she began to investigate alternative
protocols to remedy the subsequent pressure sores. Unfortunately, little had been
written on it, but she pieced together information from a variety of sources until some
common themes emerged.
Next, she assembled an interdisciplinary team of physicians, nurses and technicians to
analyze the steps involved with EEG monitoring and determine the source of
the problems.
“We began to chart best practices and asked for feedback from our
teams,” Mullen said. “That allowed us to isolate some of the problems
and come up with possible solutions.”
The first solution was to change the type of cleanser technicians used before attaching
the electrodes. In the past, technicians applied an abrasive cleanser and thoroughly
scrubbed the skin. This prevented bacterial infection, but it also irritated the skin.
“Before making a switch, we tried four different types of cleansers
to see which would work best while still preserving the skin,” said
Neurophysiology Manager Wendy Morton, a skilled EEG technician.
“Then we trained our technicians in a new, gentler way of preparing the
skin for the electrodes.”
To prevent bacteria from developing, the team researched options for disposable
electrodes. They found standard electrodes, which are metal, can break down the skin
if they’re left to sit for more than two or three days. The team compared the cost of
disposable electrodes with that of the metal ones and found disposable electrodes to be
a viable option. Disposable electrodes are softer than the metal alternatives, and they
don’t require harsh adhesives. They also reduce the risk of infection from
bacterial contamination.